The Story of the Polio Vaccine
The polio vaccine trials that eventually led to the eradication of this disease in the US—and in almost all regions of the world—began 68 years ago this month. Comparing the process that led to these trials to our recent experience with vaccinations against COVID 19 makes us aware of the huge debt we owe to pioneering medical researchers of earlier eras.
History of the Disease
Unlike COVID 19, Poliomyelitis, or polio, existed in human populations for millennia before it became a serious public health concern. For most of human history, it seems to have stricken its victims rarely and randomly (some historians believe the limping gait of the Roman Emperor Claudius resulted from a polio infection in childhood). Epidemic outbreaks of polio in the US began toward the end of the nineteenth century. One of the earliest occurred in Vermont in 1894. By 1900, communities around the country experienced occasional outbreaks.
Paradoxically, the emergence of polio as a major threat to public health coincided with widespread improvements in hygiene standards. It would be decades before a connection between hygiene and polio transmission was established and explained. Researchers studying polio infection among troops in North Africa during World War II found that the local North Africans were far less susceptible to the disease than Allied soldiers who’d grown up in areas with high sanitation standards. Further study confirmed that children born where sewage systems were poor were routinely exposed to the virus at a very young age, through contaminated water. Encountering the disease while they still carried maternal antibodies to it, they usually suffered only mild symptoms, but as a result developed their own immunity.
Panic Over Localized Epidemics
In 1916, when the first epidemic of polio began in an Italian immigrant neighborhood in Brooklyn, fear of the disease spread rapidly. Polio most often affected young children, causing flu-like symptoms; but in about 1% of cases, it entered the nervous system and caused varying degrees of paralysis. The most severe infections immobilized the muscles controlling breathing, leading to death. No one yet understood how it was transmitted; some suspected flies and mosquitoes as vectors.

By the late 1940s, polio disabled over 35,000 Americans every year, and the age of its victims was rising. Disease transmission seemed to peak in late summer. Since the disease had no known cure, prevention became the focus. Contaminated water was now suspected, and worried parents forbade their children from swimming in public pools and lakes and at beaches and from drinking from public water fountains.
A Philanthropic Effort to End Polio
President Franklin Roosevelt, who had contracted polio in 1921, at the age of 39, worked with his former law partner Basil O’Connor to found the nonprofit National Foundation for Infantile Paralysis in 1938. It raised money to research a vaccine. First funded by wealthy celebrities, the Foundation became one of the first medical philanthropies supported by a wide public. It was renamed the “March of Dimes” after Americans—who feared polio more than any other disease—responded enthusiastically when singer Eddie Cantor asked them to send their spare dimes to the White House.
Numerous Scientists Work to Solve the Vaccine Puzzle
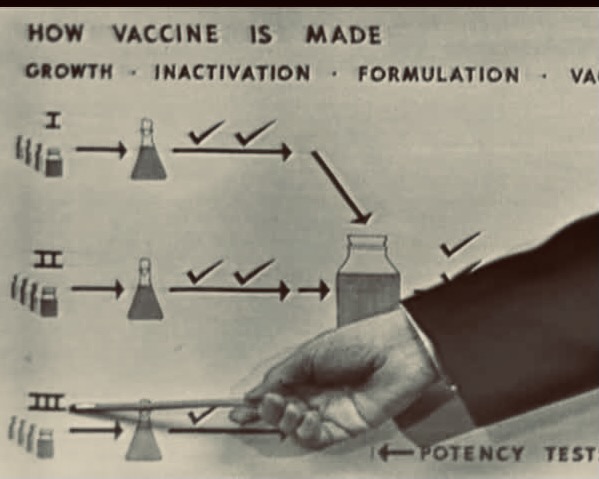
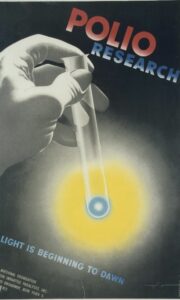
Aware that March of Dimes funding would soon be available, medical researchers who hoped to win grants began the initial vaccine work, trying to solve three problems. First, they had to determine how many strains of polio existed. A large number of researchers tackled this problem, testing dozens of samples of the virus taken from its victims. Happily, they found that all the tested strains of the polio virus fit into one of three types. Scientists then needed to develop a way of cultivating a safe, plentiful and steady supply of each the three types, so that these could be incorporated into the vaccine they developed. Three Harvard researchers—John F. Enders, Frederick C. Robbins, and Thomas H. Weller—solved this problem by finding a way to cultivate the virus in a test tube. (For this work, they won the Nobel Prize in Medicine.)
Finally, scientists needed to understand how polio made its way through the body. Only then could they feel sure a vaccine would work. Researchers had been able to isolate samples of polio virus in stool and throat cultures, and in the nerve tissue of those who died of the disease, but almost never in blood. The researcher who first traced the progress of polio in the blood was Dr. Dorothy Horstman, a female pioneer in medical research. Working with a research team at Yale, she discovered that polio ingested by mouth very quickly moved from the intestines to the bloodstream, and was very quickly destroyed by the blood’s antibody response—but not always fast enough. In some cases, the virus entered the nervous system and began causing damage before the immune response could prevent this. Scientists concluded that a vaccine could be very effective: If it tricked the blood into producing polio antibodies ahead of the initial infection, polio could be ousted from the body before it spread to the brain and spinal cord.
Live or Inactivated Vaccine?
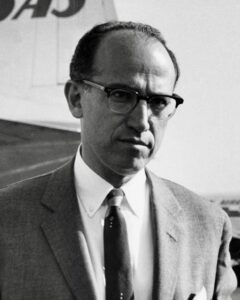
At the time, two kinds of vaccines had been developed: those using weakened doses of live virus (this was the method already used to protect people from smallpox), and those using virus that had been deactivated, or killed by applying a chemical like formaldehyde to it (such a vaccine had been developed to combat diphtheria). This first practice was considered more effective: one dose usually conferred long-term immunity. But to be safe, the vaccine had to be undergo a lengthy process of attenuation, usually by cultivating it in a series of animal tissues. The second practice was theoretically much safer, but conferred less complete immunity and could require repeated doses. One of the leading researchers competing for March of Dimes funding, Albert Sabin, pursued the live-virus vaccine approach; Jonas Salk pursued the deactivated virus approach.
Field Trials Begin
Salk’s vaccine was ready for field trials earlier than Sabin’s. With the endorsement of the March of Dimes, and funding from that organization, these began on April 23, 1954, under the direction of Salk’s former colleague, Thomas Francis of the University of Michigan, a highly respected virologist. It was one of the largest field trials ever conducted, involving two different studies with different protocols. Children in grades 1 – 3 in 84 areas in eleven states were asked to participate in one study, which was designed to satisfy scientific demands for placebo controls (half of them got the vaccine and the other half a placebo).
The other study involved over a million second graders in 127 areas in 36 states. Half of these children were vaccinated; the other half were simply “observed” as control subjects. The mixed protocol has been criticized; it was devised in an attempt to balance scientific concerns with concern for public opinion. Officials in the larger group of states were not comfortable with blinded placebo controls; they preferred to administer the vaccine to those children whose parents wanted it and simply observe the children of the vaccine-leery. Francis went ahead with trials in those states mostly as a way to prepare the public to accept it once it was approved.
A National Vaccination Campaign Begins
Francis was able to announce on April 12, 1955 his conclusion that the vaccine was 90% effective. The Eisenhower administration immediately licensed the vaccine and arranged for six pharmaceutical companies to produce it, funded at first by the March of Dimes and later through a $30 million federal grant. During 1955, each dollar of the grant paid for one child’s vaccination, and polio infection rates were halved. They would fall from 18 per 100,000 to fewer than 2 per 100,000 by the 1960s.
In Springfield, Massachusetts, Stephen Tucker and his three small children were the first to line up for the newly approved vaccine. Shortly after I met Steve—a week before I married his son David—he showed me a yellowed newspaper clipping with the headline, “Tucker Tots Get Shots.” Steve’s confidence in medical science, and zealous concern for his children, made his family role models in the local promotional effort, and he was proud of this.
Sabin’s Vaccine Overtakes Salk’s
Meanwhile, Albert Sabin continued developing a vaccine from live, weakened virus, using a mutant strain that triggered antibody production but seemed not to cause paralysis. This was tested at an Ohio reformatory, tweaked and then tested in various countries abroad before being tested in 1960 on 180,000 school children in Cincinnati, Ohio (Sabin worked at the University of Cincinnati College of Medicine). It effectively eradicated polio in that city. Sabin’s vaccine, which was administered orally, usually as a drop of red serum on a sugar cube, was fully licensed for use in the US in 1962. It was much more quickly and easily administered, and, as Sabin expected, proved even more effective than Salk’s vaccine using inactivated virus. It became the vaccine most often administered in the US for the next three decades, and was so widely given that the chain of transmission was broken. By 1979, polio was effectively eradicated in this country.
In 1988, a Global Polio Eradication Initiative was launched by the World Health Organization, a year after the Rotary Club in the US began raising money toward this purpose. Today, polio exists in only two countries: Pakistan and Afghanistan.
Both Salk and Sabin tested their vaccines on themselves and their families before testing them on other subjects. Neither Salk nor Sabin took out patents on the vaccines they developed. Both saw their work as the humanitarian answer to a pressing need.Today, Americans receive vaccinations for many communicable diseases, some using weakened live viruses, some inactivated viruses, some using only a protein that is part of a virus, and some—including two of the current vaccines for COVID 19—using the genetic code for a viral protein. Our methods for safely and rapidly producing vaccines have become much more sophisticated and reliable. We owe this progress to the thousands of researchers, vaccine trial workers, trial volunteers, and medical philanthropies who made vaccine technology a reality.
Click here for the latest worldwide polio data.